PCOS
Polycystic ovarian syndrome (PCOS) is another condition where our health industry finds itself without any good medications that can be sold to effectively manage the condition. Except for birth control, sure, why not take birth control instead of actually figuring out WTF is going wrong??? (watch Samantha Bee to maybe laugh at our sad sad system – https://www.youtube.com/watch?v=X2FS0s95o_Q )
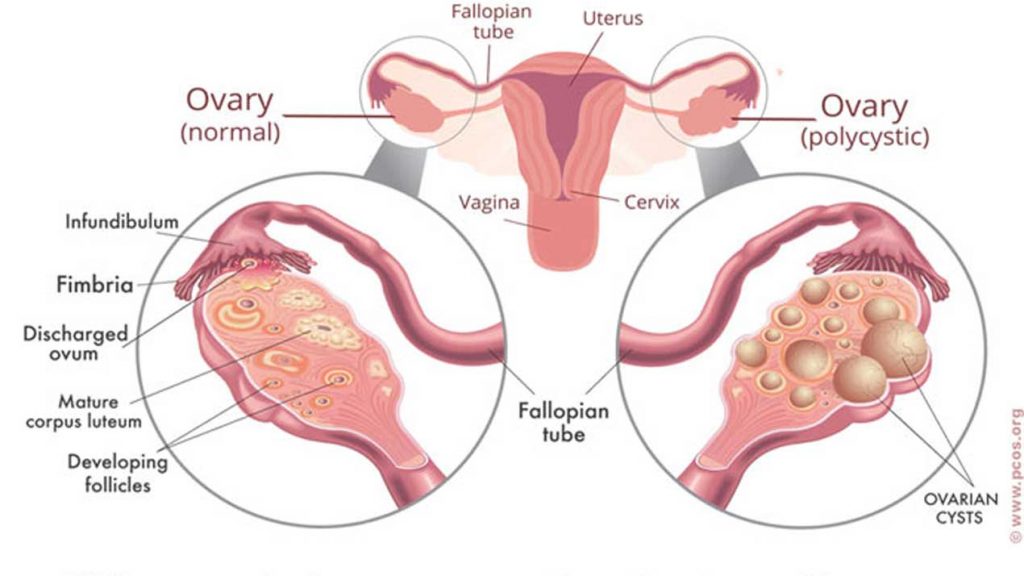
While clearly the struggle to conceive or infertility troubles may take center stage in one’s life, the impacts of PCOS go way, way beyond just that. This is one of the diseases that cluster together all being caused by metabolic syndrome (early T2 diabetes or hyperinsulinemia), which is becoming exceedingly common, but quite serious. The high insulin causing the androgen production in your ovaries will also cause damage to your arteries, increase liver fat and potential cirrhosis, gut dysbiosis and low grade inflammation, increased risk of heart attack, stroke, Alzheimers/dementia, loss of glycemic control a.k.a. T2 diabetes (leading to many potential organ and tissue damage, blindness, amputations), and even many types of cancer.
Oh right, lets not forget that if you do manage to get pregnant, but have not resolved the high insulin, then you will be at much greater risk for many potential complications, such as miscarriage, preeclampsia, premature birth, and other fun stuff. See here for more: https://www.nichd.nih.gov/health/topics/pcos/more_information/FAQs/pregnancy
If we stop to better understand why and how this condition progresses, then we actually learn some techniques that may help to better manage it. Similar to type 2 diabetes, PCOS is also a disease of metabolic derangement.
For the general understanding of PCOS, I am going to refer mostly to IDM program’s blog (Dr. Jason Fung and his team – in this case Dr. Nadia). They are the primary ones that I have seen address the underlying causes of this condition (although I haven’t yet looked all that hard elsewhere, maybe someone else has good info too?), so they are a good place to start.
To the best of my understanding, two of the biggest contributors to this problem are high insulin (insulin resistance) and too much growth signaling (mTOR). You can find plenty of info on mTOR and mTORC1 modulation/dampening in some scholarly articles and some good nerdy videos, but you got to be ready for that crap or it will put you to sleep. The basics principal is that to control insulin, we need to greatly reduce processed carbohydrates, starches, and especially sugars – fructose being one of the worst offenders to the liver; and to control mTOR, lowering insulin is huge, but reducing amino acid availability is also required, so basically water-only fasting becomes an ideal tool (provided you are not pregnant).
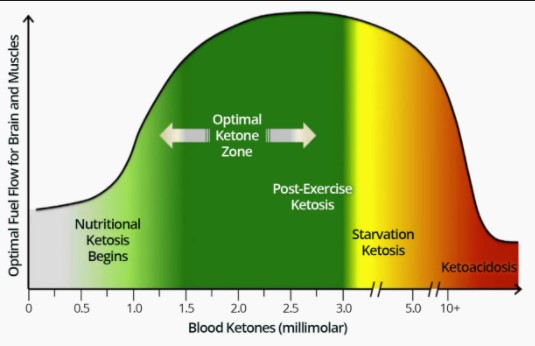
Now if you are a big fan of pharmaceuticals, than metformin may be a good place to start, but fortunately these two birds are killed with the same stone naturally. The best tools being low carb higher fat diets (such as ketogenic), periodic fasting, and time-restricted eating. Now, you could pick one and go with it, and maybe get sufficient results, but if you combine all three, now you are cooking with fire, and will get where you want to be much quicker and stay there much more easily. A strict therapeutic ketogenic diet can be difficult to maintain, but if you restrict your eating window to 6-8 hours a day (with last food at least 3-4 hours before bedtime), then you will likely be able to eat a bit more protein and some healthy carbs (i.e. unprocessed) and still maintain a high enough state of ketosis. Myself, I just skip breakfast, eat a large lunch at about 1pm, and a small dinner (usually by 7 or 8 pm).
First and foremost, sugar and processed carbs must be greatly reduced from daily consumption. Start off by counting how many grams of sugar a day you are eating. Then cut it in half. This could mean eating half portions of your treats or eating them half as often. After a few weeks, cut it in half again, and again, until you get down near 10 grams a day most days. If you go too fast it will be harder, but don’t drag it out too long either, because you got somewhere you want to be. This gives your body time to adjust and ween yourself off of this need for constant sweetness. My brain gave me a very hard time, especially after lunch. I wasn’t hungry, but I wanted my sugar fix. I was addicted since a young child, but now I get very little pleasure out of sweets, and can’t even eat much if I wanted to.
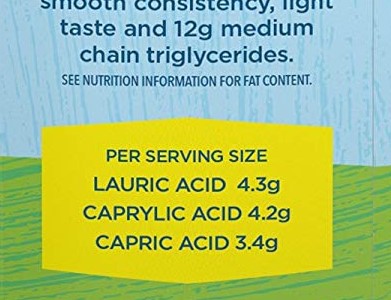
Fake sweeteners? Just don’t! Some will still spike insulin if eaten with food, some have been shown to negatively impact gut bacteria, so they certainly are going to do something in your body. My personal thought is this – it’s your brain asking for this glucose bump, and if you eat fake sugar, well, you taste sweetness, but your brain is still at the door waiting for the package to be delivered. It knows it didn’t get it, and will ask again. Slowly take that away, and it will quit asking for so much. If you order an item online, and it never comes, eventually you are going to wonder where the hell it is, and maybe order it again from somewhere else. Don’t think that your brain is that stupid that you can fool it with fake sugar. My hypothesis is that cravings are mostly driven by a reduction in available brain energy, and my quick fix is to eat butter (in the context of low insulin) and MCT oil (processed coconut) in order to compensate. So far it has worked quite well for me.
Throw in a 24hr fast once every week or two, and you may find that it’s really not that hard to do. Now it’s nothing that I really look forward to, so I find it helpful to designate a day (say Monday or whatever) because otherwise it’s just too easy to not do it. A 24 hour fast is really pretty easy as long as you don’t mind-block yourself before trying it. Many people just think “I could never do that”, but in reality, it isn’t all that difficult. Wake up, don’t eat breakfast, don’t eat lunch, enjoy your well-deserved dinner. Congratulations, you made it! In my experience, the feeling of hunger only lasts 10 minutes or so at a time, so if you can ignore it for a bit, it will go away for a while. A cup of black coffee or plain tea can do wonders to kill hunger. If you are really motivated, then push the fast duration up to 36 or 48 hours, and eventually 3-5 days if you can. Personally, I aim to do a 3-7 day fast at least a couple times a year for the multiple benefits, especially in relation to cancer prevention, but so far the only longer fasts that I’ve managed are one 3-day and one 4-day fast. It’s much harder to pull off with family life if you are the only one doing it. If you are really metabolically deranged and want to hurry things along, then you may want to do more frequent 2-7 day fasts from the start. I’ve heard its not much fun if you are not fat/ketone adapted, but its certainly an effective way to speed things along in the recovery. And fasting is a powerful tool in recovering insulin sensitivity, autophagy, and mitochondrial rejuvenation. All good things.
Obviously exercise is another great tool for improving insulin sensitivity. While HIIT or high-intensity interval training is getting pretty popular, in reality, low-intensity long-duration exercise is said to be great for improving mitochondrial health and reducing the amount of insulin required to maintain glucose levels, a.k.a. improving insulin sensitivity. This should be a brisk walk for most people, something that lets them maintain conversation without getting short of breath. For a deep discussion of this exercise and mitochondria topic see Peter Attia’s podcase episode #85 –https://peterattiamd.com/inigosanmillan/
IDM Program – Looks like they have quite a few parts now:
intro – https://idmprogram.com/fasting-polycystic-diseases/
1) https://idmprogram.com/the-faces-of-polycystic-ovary-syndrome-pcos/
2) https://idmprogram.com/diabetes-of-bearded-women-pcos-2/
3) https://idmprogram.com/hyperandrogenism-pcos-3/
4) https://idmprogram.com/differential-diagnosis-pcos-4/
5) https://idmprogram.com/pcos-and-obesity-pcos-5/
6) https://idmprogram.com/pcos-and-associated-condition-pcos-6/
7) https://idmprogram.com/pcos-and-hyperandrogenism-pcos-7/
8) https://idmprogram.com/pcos-and-hyperinsulinemia-pcos-8/
9) https://idmprogram.com/pcos-anovulatory-cycles-and-hyperinsulinemia-pcos-9/
Looks like Nadia and Fung have a new book coming out in May https://www.amazon.com/PCOS-Plan-Prevent-Polycystic-Syndrome/dp/1771644605/
See her short interview with Ivor Cummins for a brief background: https://www.youtube.com/watch?v=ijn6ICTIJVM
————————————————————-
Discussion from 2009 – Diana McNeill, MD and Ann J. Brown MD MHS
https://www.youtube.com/watch?v=ABGVgpbW9Iw&t=357s
Very good overview – knowledgeable understanding of the disease, and much more detail on other aspects and issues.
IR at the center of treatability – lifestyle most effective approach.
Discussion of testosterone testing and limitations.
Apparently unaware of the potential effectiveness of fasting. I guess in 2011 it was not all that embraced as a medical tool. Fasting has many mechanisms of action, probably many still unknown, but definitely minimizes insulin and greatly dampens mTOR activity.
I recall Dr Peter Attia had noticed his testosterone nosedived during a 1 week fast. Not sure if this would occur in women as well, and if it did, could shorter more frequent fasts be an effective means to maintain lower T?
—————————————————————
Understanding a little bit about mTOR can help to tie all of this together a bit.
Michael Hall (University of Basel): The Story of TOR (Target of Rapamycin) https://www.youtube.com/watch?v=VYVjE6HEgy0
David Sabatini (Whitehead, MIT, HHMI) 1: Introduction to mTOR and the Regulation of Growth https://www.youtube.com/watch?v=EnIerDljc7g
—————————————————————–
Links for ketogenic diet help:
Check out my page on ketogenic diets for an overview and good keto links – https://revhealthhub.com/ketogenic-diets/
Dominic D’Agostino’s site – many resources for keto diet, and also many great video interviews exploring other aspects of ketone physiology.
https://www.ketonutrition.org/practical-guides-to-the-ketogenic-diet
And in terms of better understanding metabolism, I would always recommend Dr. Jason Fung’s books The Obesity Code, and the Diabetes Code.