Gallbladder concerns?
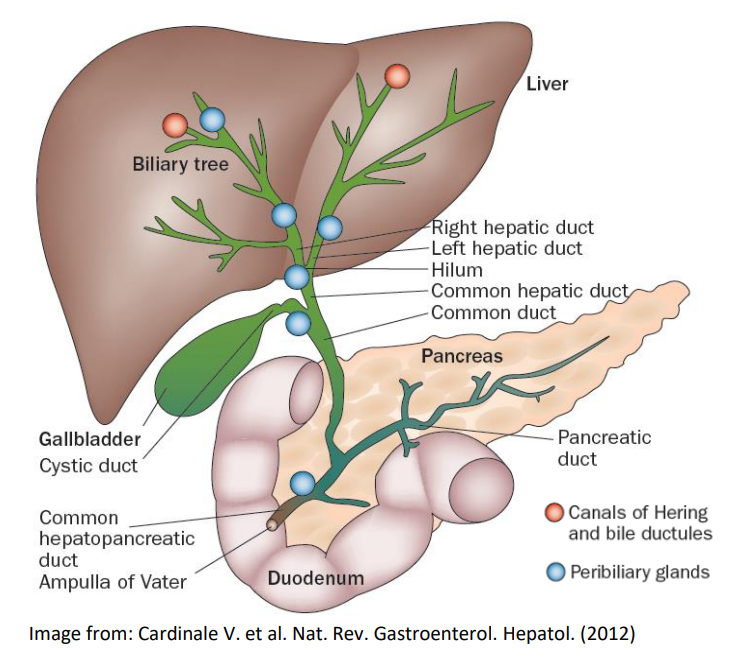
When I first started getting into the whole high fat diet, this thought popped into my head “What about gallstones?” I’ve never had issues myself, but I know people who have, and the typical advice they were given was to avoid a fatty diet to avoid problems. If people are so well adapted to eating fats for energy, then surely there must be some kind of big misunderstanding here as well. Absolutely! A terrible misunderstanding of the nature of the problem. So as brief and simple as I can put this: the gall bladder stores bile acids (made by the liver) that assist in digestion and absorption of dietary fats. The purpose of bile is to help digest fat, so how can anyone explain how using bile for what it was intended could cause stone formation? It just sounds stupid because it is! However, when we eat a low-fat diet, we don’t need as much, so by decreased use, the pool of bile acids sit around stagnant and concentrates in the gallbladder. Crystallizations begin to occur, which eventually result in the formation of sludge and/or gallstones. (Clinical study – https://www.nature.com/articles/0800634) So now that you have managed to form these stones by eating too little fat, and have them already present, sitting in your gallbladder, NOW if you do suddenly eat a very fatty meal, your gallbladder activates with a strong response, pushing these crystallizations/stones into the narrow passageways in route to your GI, causing obstruction and sometimes complete blockage. Here are a couple sites that explain it fairly well, but there are numerous others out there as well if you need more convincing: https://www.dietdoctor.com/gallstones-and-low-carb, https://www.atkins.com/how-it-works/library/articles/dealing-with-gallbladder-disorders.
Full stop! – That was the overly-simplified explanation that already seemed more plausible than the traditional view, but it still didn’t complete the puzzle. It also didn’t provide too much for ways to make a meaningful impact on risk aside from liver health. Realistically it has to be something more than simply stagnation and lack of use, but rather some biochemical event must be changing the tendency of the bile to produce or not produce stones.
While a very low-fat diet seems to promote gallstone formation, not eating anything at all (a.k.a. fasting) does not cause any substantial risk of gallstone formation in most people, so clearly some biochemical change must occur that lowers the solubility of the bile salts and cholesterol. Additionally, some people manage to get gallstones despite eating plenty of fats, and stone formation tends to correlate with metabolic syndrome (hyperinsulinemia), and is also higher with celiac damage, so clearly there are multiple pathways and contributing factors. Stones can also form in the common bile duct, gallbladder or not, so nothing to do with stagnation there. This sent me out in search of some sort of explanation to make sense of these inconsistencies. I eventually found a brief mention in a decades old abstract – that phosphatidylcholine (PC) and oxysterols in combination help stabilize bile and prevent crystallization, which seemed pretty important to me. I am assuming that oxysterols are less likely to be in short supply, and that PC is more deserving of our attention. A number of other papers seem to confirm that increased PC correlates with lower stone incidence as well.
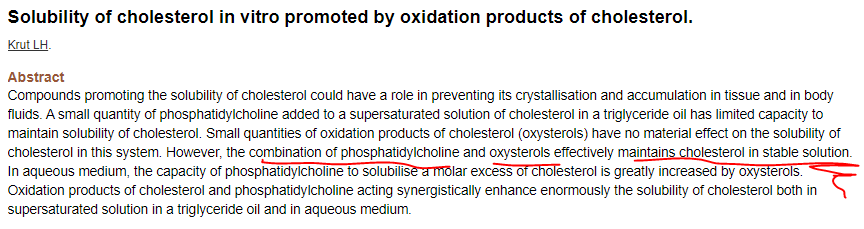
So let’s see, choline deficiency will cause fatty liver (obstructs bile production/flow), and not enough choline may result in the body stressed to produce enough phosphatidylcholine, which could then decrease the solubility of the bile within the gallbladder, resulting in stone formation. Maybe we want to avoid choline/betaine deficiency!!! (Side note – its going to be much more difficult to get sufficient choline/betaine on a low-fat diet).
The pathways of choline and folate are intertwined, both help power methylation, which is needed to maintain SAM (s-adenyl-methionine), and proper SAM supply is needed for PC synthesis, creatine synthesis, regulation of anti-oxidant glutathione production, etc. Folate deficiency or MTHFR mutations can cause a much greater need of choline/betaine, so both are capable of causing imbalance.
I personally go out of my way to get more choline in my diet and add plenty through supplementation as well, although I do have SNPs downregulating both MTHFR and choline pathways, so that may not be all that necessary for everyone. Oh, and seriously doubling up the egg yolks in some scrambled eggs is super tasty! (Secret to good eggs – just add lots of butter and don’t overcook them or burn the butter.)
Interesting note – “phosphatidylcholine led to an improved clinical activity index” for ulcerative colitis, meaning it decreased the severity of disease symptoms. https://doi.org/10.1080%2F00365521.2017.1326163 I’m guessing that an increase in bile flow had something to do with the improvement in disease status, as well as PC playing an important role in the intestinal glycocalyx/mucosa (gut barrier layer) antibacterial protection (https://www.sciencedirect.com/science/article/pii/S0005273617300627). Sufficient bile helps promote overall GIT health, as well as improved absorption of fat-soluble vitamins such as A, D, E, and K. And yes, fat-soluble means eat your veggies with some sort of fat to maximize absorption of these nutrients.
People who develop gallstones despite eating plenty of fat may have choline deficiency issues and/or liver dysfunction, or might be celiac (diagnosed or not), or possibly some other mechanism is at play. Whatever it may be, eating too much fat is almost certainly not the cause.
As briefly mentioned above, in celiac afflicted individuals consuming gluten, gastro-intestinal tract (GIT) damage in the duodenum can cause sensory cells that normally should trigger contraction of the gallbladder in the presence of fats to become damaged, resulting in a muted, sluggish, or dysfunctional contraction response, and thereby decreased bile ejection. Bile serves many functions in maintaining proper absorption, as well as GIT lubrication and microbiome moderator, so decreased bile surge is likely to exacerbate an already damaged GIT that is a hallmark of celiac disease.
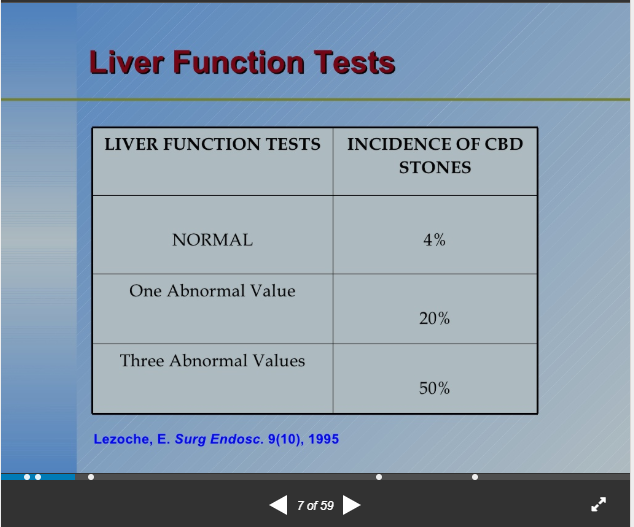
Liver health is another big factor in the formation of gall stones. Your liver is the organ that produces bile, which is then concentrated and stored in the gall bladder. If someone develops liver disfunction (which could be caused by fatty liver due to excess fructose, hyperinsulinemia, 1-carbon metabolism imbalance, alcohol, etc.), then it may not be able to make sufficient bile, or thyroid hormone, both of which can affect stone formation and also leads to a number of different problems. Amino acids taurine and glycine are precursors to bile salt formation, so supplementation may be helpful to ensure deficiency isn’t impeding production. The slide below is from a powerpoint I found on the web, most of which was a little too specialized to be helpful for me, but slide 7 struck note – notice the risk of stone formation is huge for those with three abnormal liver function values. I was going to say 10 times higher, but that doesn’t really capture the magnitude of the increased risk, which afflicted HALF of the group with 3 abnormal values. It went from 4/100 to 50/100, so yeah, the liver is a big player here.
Systems in our body are not independent, but rather they are intertwined. The liver, thyroid, gall bladder and GI all affect each other, and they do so in both directions, so problems in one system will lead to other systems dysfunction as well. Liver problems may not be as noticeable, but might still be impacting the health of other systems in ways that we do notice. The liver is responsible for creating/converting a large percentage of thyroid hormone, so liver disfunction will impair this task, and people with hypothyroid issues have an increased risk for bile problems and common bile duct stone formation. So yes, it’s complicated, but if you can avoid giving yourself a fatty liver by fixing insulin resistance issues, minimizing fructose consumption, and avoiding choline deficiency, then there is less chance of things getting pushed out of balance, and recovering liver function may even help bring thyroid and other systems back into balance.
If you do get your gallbladder removed, it isn’t any more dangerous to continue eating fats, but you will be less able to metabolize fats and will be less efficient in absorbing fat-soluble nutrients. Doctors and hospitals may want to remove your gallbladder due to their failure to understand its importance, and because they get to charge you a lot of money to do so. I’ll let you decide which of those two factors weighs in heavier on their decision, but if it were me, I would tell them that we need to focus on increasing bile production and dissolving the stones, and to leave the organ where it belongs (provided that it is otherwise healthy) since it is far from a useless organ. Also, getting your gallbladder removed doesn’t eliminate the possibility of stone formation within the biliary tree and common bile duct. To do that, it would take actual lifestyle changes to reduce that risk.